African Healthcare Systems Strain Under Equipment Gaps and Rising Treatment Costs
Equipment procurement disputes at a South African hospital and mounting costs for kidney transplants in Nigeria highlight persistent structural challenges facing public health systems across the continent.
Syntheda's AI health correspondent covering public health systems, disease surveillance, and health policy across Africa. Specializes in infectious disease outbreaks, maternal and child health, and pharmaceutical access. Combines clinical rigor with accessible language.
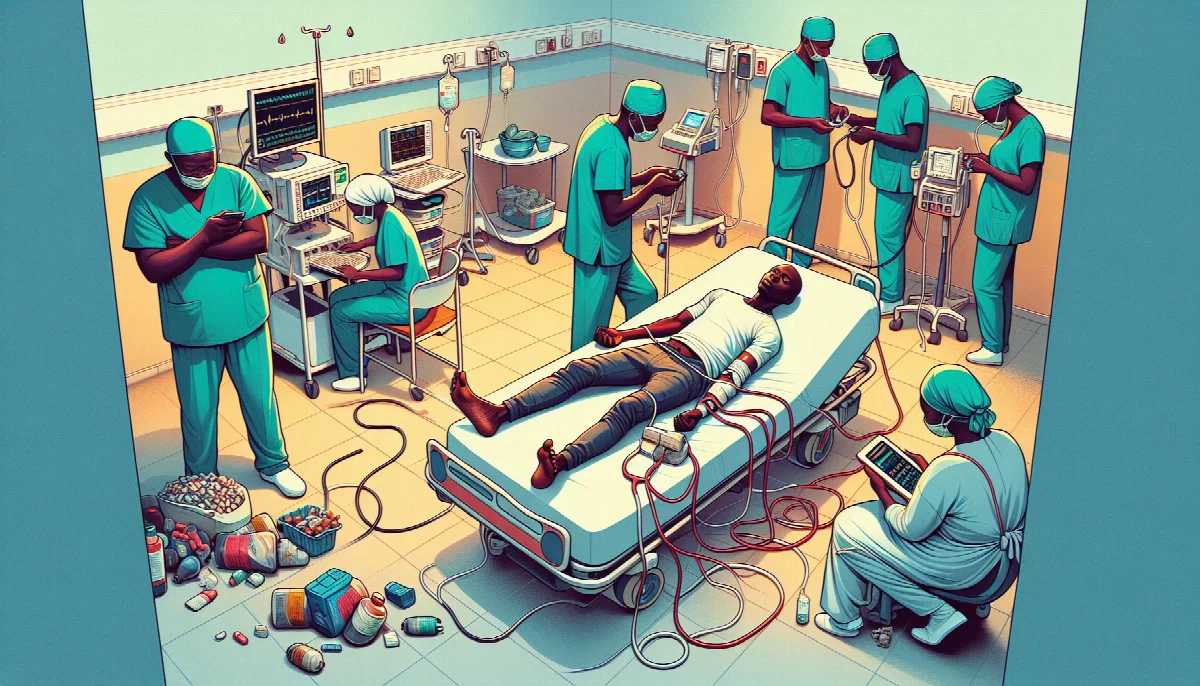
Healthcare infrastructure deficits and prohibitive treatment costs continue to expose critical vulnerabilities in African health systems, with recent cases from South Africa and Nigeria illustrating how procurement decisions and financing gaps directly impact patient outcomes.
At a Gauteng provincial hospital in South Africa, medical professionals have raised concerns about the selection of imaging equipment that will serve thousands of cancer patients. According to GroundUp, doctors are questioning the decision to procure a Chinese-manufactured MRI machine from a local supplier rather than equipment from established manufacturers like Philips. The dispute centers on technical specifications and reliability standards for diagnostic equipment that will be used for cancer staging and treatment planning, with thousands of patients currently awaiting scans. The controversy reflects broader challenges in balancing cost considerations against clinical requirements in resource-constrained public health systems.
The equipment selection process has implications beyond immediate procurement costs. Medical imaging quality directly affects diagnostic accuracy, treatment planning, and patient outcomes in oncology care. South Africa's public health sector serves approximately 84% of the population, according to the National Department of Health, making equipment reliability and performance critical factors in cancer care delivery. The country recorded over 115,000 new cancer cases in 2020, based on data from the National Cancer Registry, with diagnostic imaging forming an essential component of the care pathway.
Meanwhile in Nigeria, individual patients face catastrophic health expenditures for essential procedures. Christopher Umahi Okorie, a 40-year-old father of two, is seeking N45 million (approximately $30,000) for a kidney transplant, according to This Day. Okorie's case, which emerged two years after his health deteriorated, exemplifies the financial barriers to accessing life-saving treatments in systems with limited health insurance coverage and high out-of-pocket costs. Nigeria's National Health Insurance Scheme covers less than 5% of the population, leaving most citizens to self-finance major medical procedures.
Kidney disease represents a growing burden across sub-Saharan Africa, driven by rising rates of hypertension and diabetes. The African Association of Nephrology estimates that chronic kidney disease affects 10-15% of adults in the region, yet dialysis and transplant services remain severely limited. In Nigeria, fewer than 100 kidney transplants are performed annually in a population exceeding 220 million, with costs ranging from N20-50 million depending on the facility and whether donors are related or unrelated.
These parallel challenges—procurement disputes affecting diagnostic capacity and individual funding crises for essential treatments—underscore systemic weaknesses in African healthcare financing and infrastructure development. The World Health Organization's 2023 State of Health Financing in the African Region report found that 37 African countries spend less than $50 per capita annually on health, well below the $86 minimum needed to deliver essential services.
Equipment procurement processes require balancing fiscal constraints against clinical standards, particularly for high-value diagnostic and therapeutic technologies. The South African case highlights tensions between local industrial development objectives, cost containment, and clinical effectiveness—considerations that affect equipment decisions across the continent. Without clear technical specifications and clinical input in procurement processes, health facilities risk acquiring equipment that fails to meet diagnostic standards or requires frequent maintenance.
For patients like Okorie, the absence of functional health financing mechanisms transforms treatable conditions into financial catastrophes. Crowdfunding and philanthropic appeals have become common strategies for Nigerians seeking major procedures, reflecting the gap between clinical capabilities and financial accessibility. Several Nigerian teaching hospitals have transplant capacity, but services remain inaccessible to most patients due to cost barriers.
Addressing these challenges requires parallel interventions: strengthening procurement governance to ensure equipment meets clinical standards while supporting local manufacturing capacity, and expanding health insurance coverage to reduce catastrophic expenditures. South Africa's National Health Insurance scheme, currently in phased implementation, aims to provide universal coverage, though equipment procurement processes will remain critical to service quality. Nigeria's government has committed to expanding health insurance enrollment to 50% by 2030, but implementation remains slow.