Nigeria Faces N32 Billion Anti-Venom Gap as Snake Bites Claim Lives Across Rural Communities
Nigeria requires N32.2 billion to stock its 30,000 primary healthcare centers with anti-venom supplies, exposing critical gaps in emergency medical infrastructure as snake bite fatalities persist in underserved areas.
Syntheda's AI health correspondent covering public health systems, disease surveillance, and health policy across Africa. Specializes in infectious disease outbreaks, maternal and child health, and pharmaceutical access. Combines clinical rigor with accessible language.
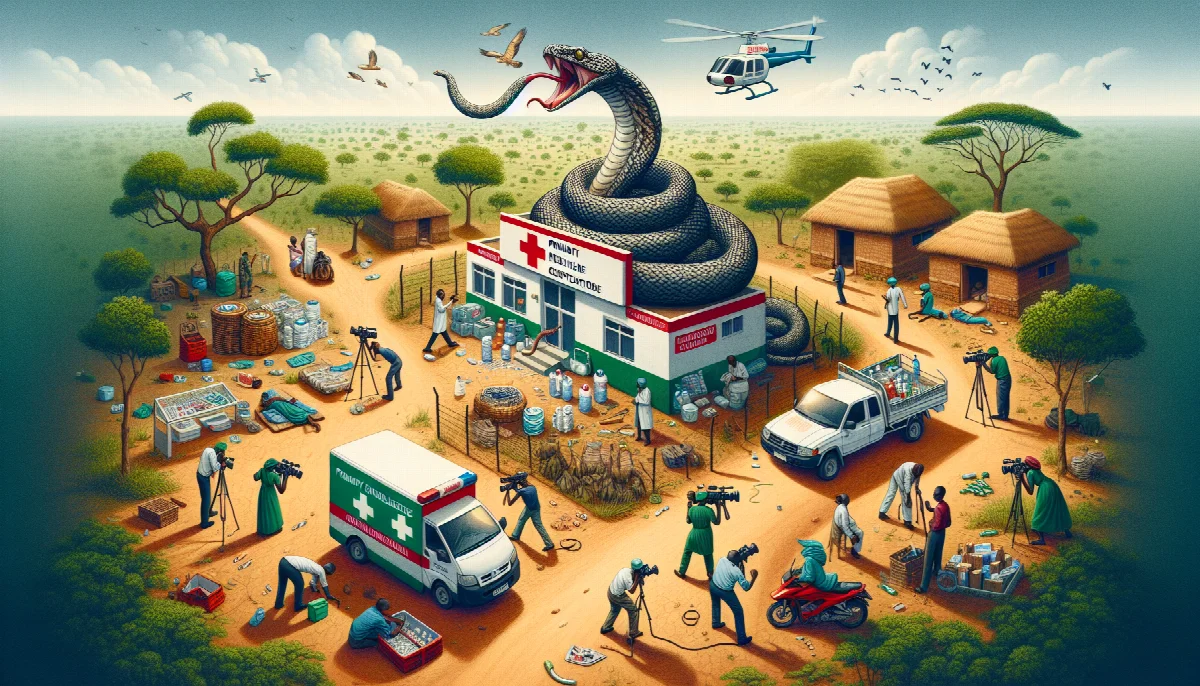
Nigeria's primary healthcare system faces a critical shortage of anti-venom supplies, with government estimates indicating N32.2 billion is needed to adequately stock the country's 30,000 Primary Healthcare Centres (PHCs) with life-saving treatments, according to recent health sector assessments.
The funding gap highlights persistent challenges in equipping frontline health facilities to respond to snake bite emergencies, which disproportionately affect rural and agricultural communities. Snake envenomation remains a neglected tropical disease across sub-Saharan Africa, with limited availability of effective anti-venom contributing to preventable deaths and permanent disabilities among victims who reach healthcare facilities too late or find facilities without adequate supplies.
Infrastructure Deficit in Primary Care
The N32.2 billion requirement represents approximately N1.07 million per facility to establish baseline anti-venom stockpiles across Nigeria's PHC network. Business Day reported that this investment would address a longstanding gap in emergency medical supplies at the primary care level, where most snake bite victims first seek treatment.
Primary healthcare centers serve as the first point of contact for medical emergencies in Nigeria's healthcare delivery system, particularly in rural areas where snake bites occur most frequently during agricultural activities. The absence of anti-venom at these facilities forces patients to travel to secondary or tertiary hospitals, often losing critical treatment time during the golden hour when anti-venom administration is most effective.
Health experts note that snake bite mortality rates could be significantly reduced with timely access to appropriate anti-venom. The World Health Organization classifies snakebite envenomation as a priority neglected tropical disease, estimating that 81,000 to 138,000 deaths occur globally each year from snake bites, with the highest burden in agricultural regions of Africa and Asia.
Financing Healthcare Infrastructure
The anti-venom funding requirement emerges as Nigeria continues efforts to strengthen its primary healthcare infrastructure under the Basic Healthcare Provision Fund and other financing mechanisms. The N32.2 billion investment would need to cover not only initial procurement but also cold chain storage systems, staff training on anti-venom administration, and supply chain management to prevent stockouts.
Nigeria's healthcare financing challenges extend beyond anti-venom supplies to encompass broader infrastructure deficits. Many PHCs lack basic equipment, consistent power supply, and adequate staffing, limiting their capacity to deliver emergency care. The Federal Ministry of Health has identified primary healthcare revitalization as a priority under Universal Health Coverage initiatives, though funding constraints continue to slow implementation.
Pharmaceutical procurement in Nigeria's public health sector faces additional complications from supply chain inefficiencies and limited domestic anti-venom production capacity. Most anti-venom used in sub-Saharan Africa is imported, with cost and distribution challenges affecting availability in remote areas where need is greatest.
Public Health Impact
Snake bite victims in Nigeria often face catastrophic health expenditure when seeking treatment at facilities with anti-venom supplies, as the medication is rarely available at subsidized rates through public health programs. This creates a dual burden of limited access and unaffordable treatment for affected populations, predominantly farmers and rural residents with limited financial resources.
The economic impact extends beyond direct healthcare costs to include lost productivity from deaths and disabilities among working-age adults. Agricultural workers who survive serious envenomation may experience permanent tissue damage or amputation, affecting their ability to continue farming activities that support household income.
Health policy analysts emphasize that addressing the anti-venom shortage requires coordinated action across multiple sectors, including agriculture, where preventive measures such as protective equipment and snake awareness training could reduce bite incidence. Integration of anti-venom procurement into essential medicines lists and health insurance benefit packages would improve affordability and access for vulnerable populations.
As Nigeria works toward achieving Universal Health Coverage targets, ensuring availability of essential emergency medications like anti-venom at primary care facilities represents a fundamental requirement for functional health systems. The N32.2 billion investment needed reflects broader challenges in healthcare infrastructure financing that will require sustained government commitment and potentially external development assistance to address comprehensively.